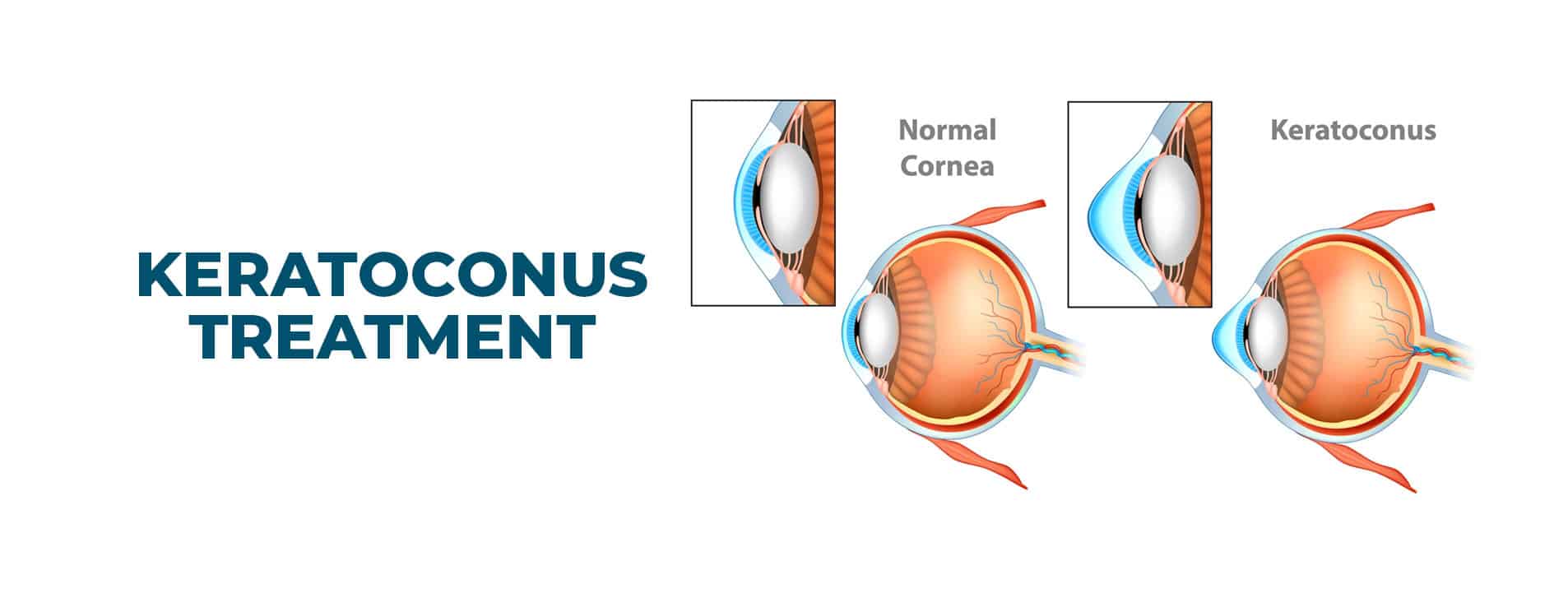
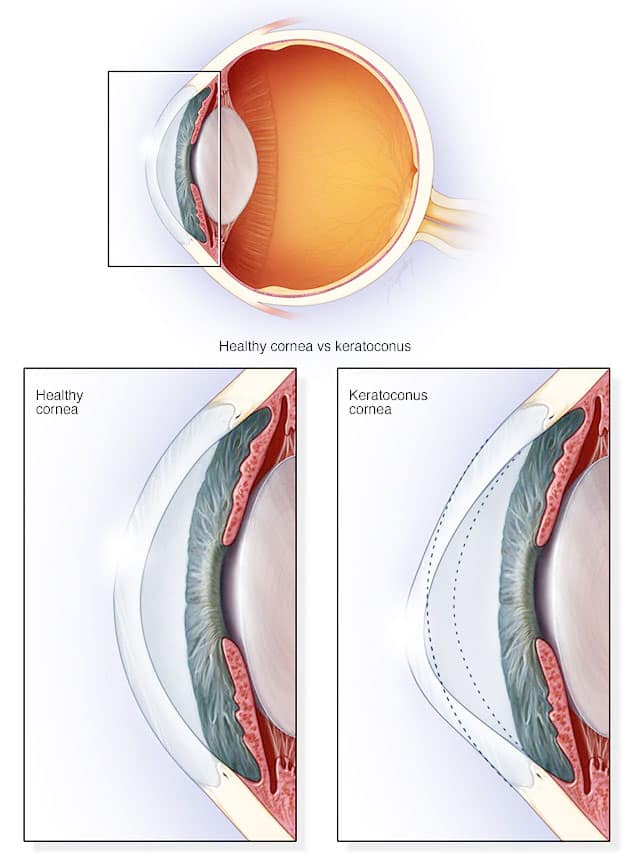
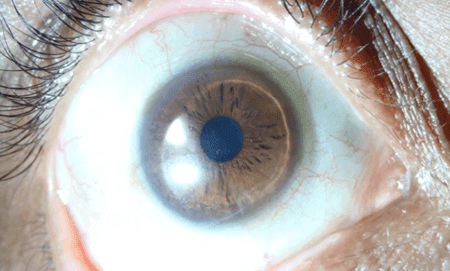
Keratoconus is a disorder of the eye due to the gradual thinning and bulging of the central portion of the cornea in a conical shape. It is associated with significant visual problems like blurring and distortion of vision, increased sensitivity to light etc. Early stages are treatable with glasses while corneal transplantation is required for advanced stages to restore vision.
The Centre of Excellence for Keratoconus @Narayana Nethralaya is equipped with the most advanced technologies available in the world for diagnosing, evaluating and treating all forms of Keratoconus and with Dr Rohit Shetty at its helm is a pioneer in the field of Keratoconus Research and Genetics. Dr Rohit Shetty holds an international PhD(Netherlands) for his extensive work in Keratoconus, and along with his team of scientists is responsible for many path breaking discoveries including discovering new genes responsible for the disease, establishing and treating Keratoconus as an inflammatory disorder and newer Surgical Laser Treatment modalities which are now being followed all around the world.
Narayana Nethralaya’s Journey in the field of Keratoconus Research began in the later half of the first decade of 2000 while the world still believed that Keratoconus was a noninflammatory and degenerative disease without a well understood pathogenesis. The department on an average sees …….patients from all over India and performs …… Keratoconus related surgeries every year. These patients stand as testimony and brand ambassadors to the quality of care offered at NN.
Keratoconus is a relatively rare disease with prevalence estimates ranging from 4 per 100,000 people to 600 per 100,000 with prevalence about equal between males and females. A disease that mostly begins at puberty, it progresses far into the mid-30s, developing in both eyes in majority of cases, though the rate of progression and the timing of the onset of Keratoconus may vary with each eye.
With Keratoconus, the cornea thins and bulges into an irregular cone shape, resulting in vision impairment. In the cornea, the middle layer is the thickest part of the cornea, mostly made up of water and a protein called collagen. Collagen gives the cornea its strong and flexibility. This healthy cornea focuses light so you can see clearly.
Causes of Keratoconus
Despite our long experience with this long chronic disease, the causes are mostly unknown. The weakening of collagen fibrils causes the cornea to bulge out in the form of a cone.
According to new research, an imbalance of enzymes can cause this disease, which can make the cornea more susceptible to oxidative damage by free radicals, making it weak and bulge outwards.. Keratoconus is caused by a decrease in these enzymes and protective antioxidants in the cornea.
Some risk factors can increase the chances of someone being affected. These include:
Heredity—chances of developing Keratoconus increases if any of your family member is affected
Overexposure to ultraviolet rays
Poorly fitted contacts
Eye Allergies and chronic eye rubbing-Chronic eye rubbing is associated with developing keratoconus. It may also be a risk factor for disease progression.
Certain diseases, including retinitis pigmentosa, atopic disease and connective tissue disorders.
Down Syndrome
Diagnosis of Keratoconus
To diagnose Keratoconus, we will review your medical and family history and conduct an eye exam. This also involves other tests to determine more details regarding the shape and strength of your cornea.
Eye refraction
We have specially trained optometrists who will use special equipment to check for the right combination of lenses to give you the sharpest vision.

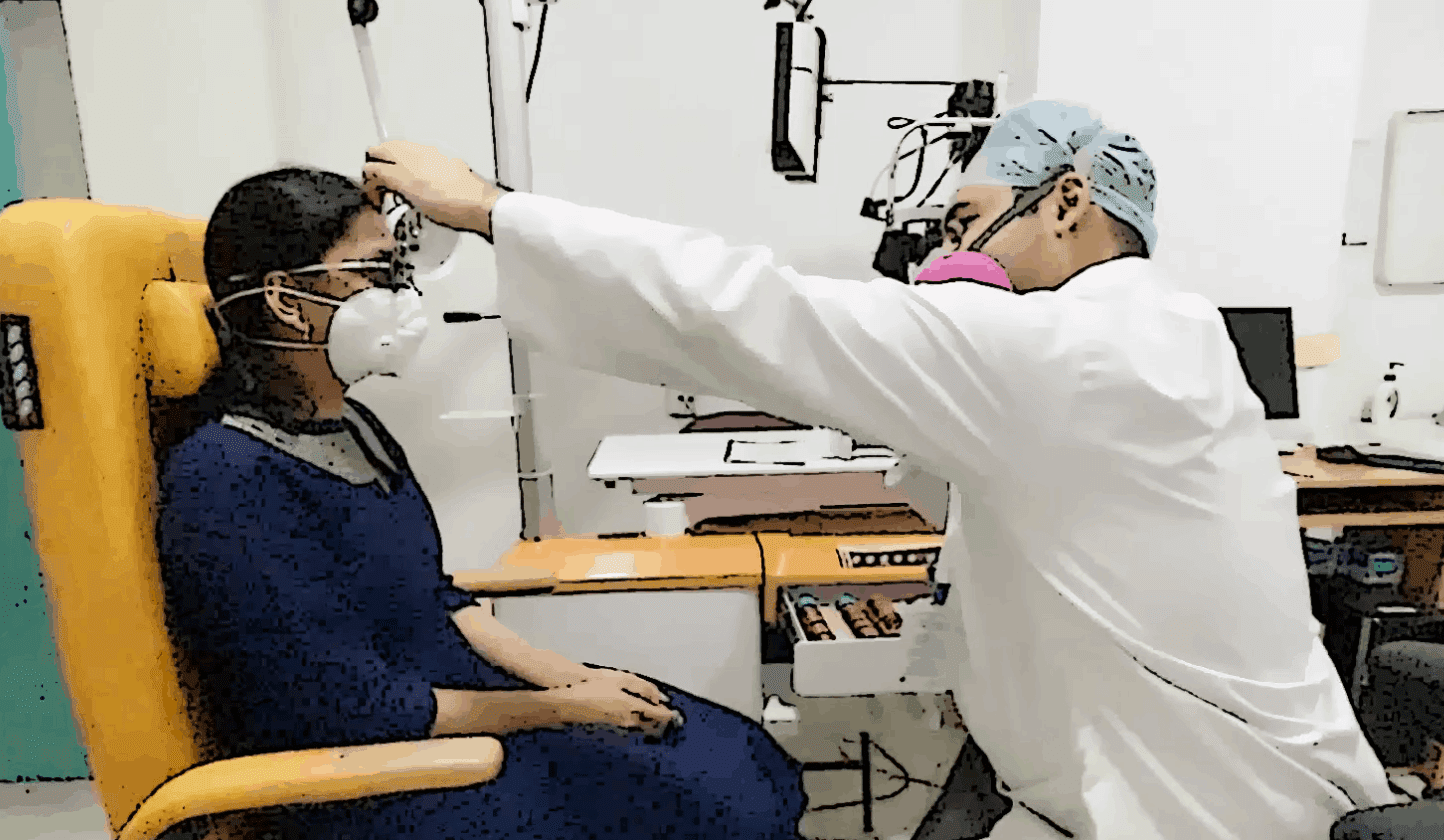
Slit-lamp examination
A vertical beam of light is used on the surface of your eye through a low-powered microscope to view your eye. He or she evaluates the shape of your cornea and looks for other potential problems in your eye like allergy etc which have a strong association with keratoconus.

Computerized corneal mapping
Advanced diagnostic tests, such as optical coherence tomography and corneal topography, record images of your cornea to create a detailed shape map of your cornea’s surface, as well as measure the thickness of your cornea. We also have advanced equipments that help measure the strength of your cornea.
Advanced Diagnostics – All under one roof
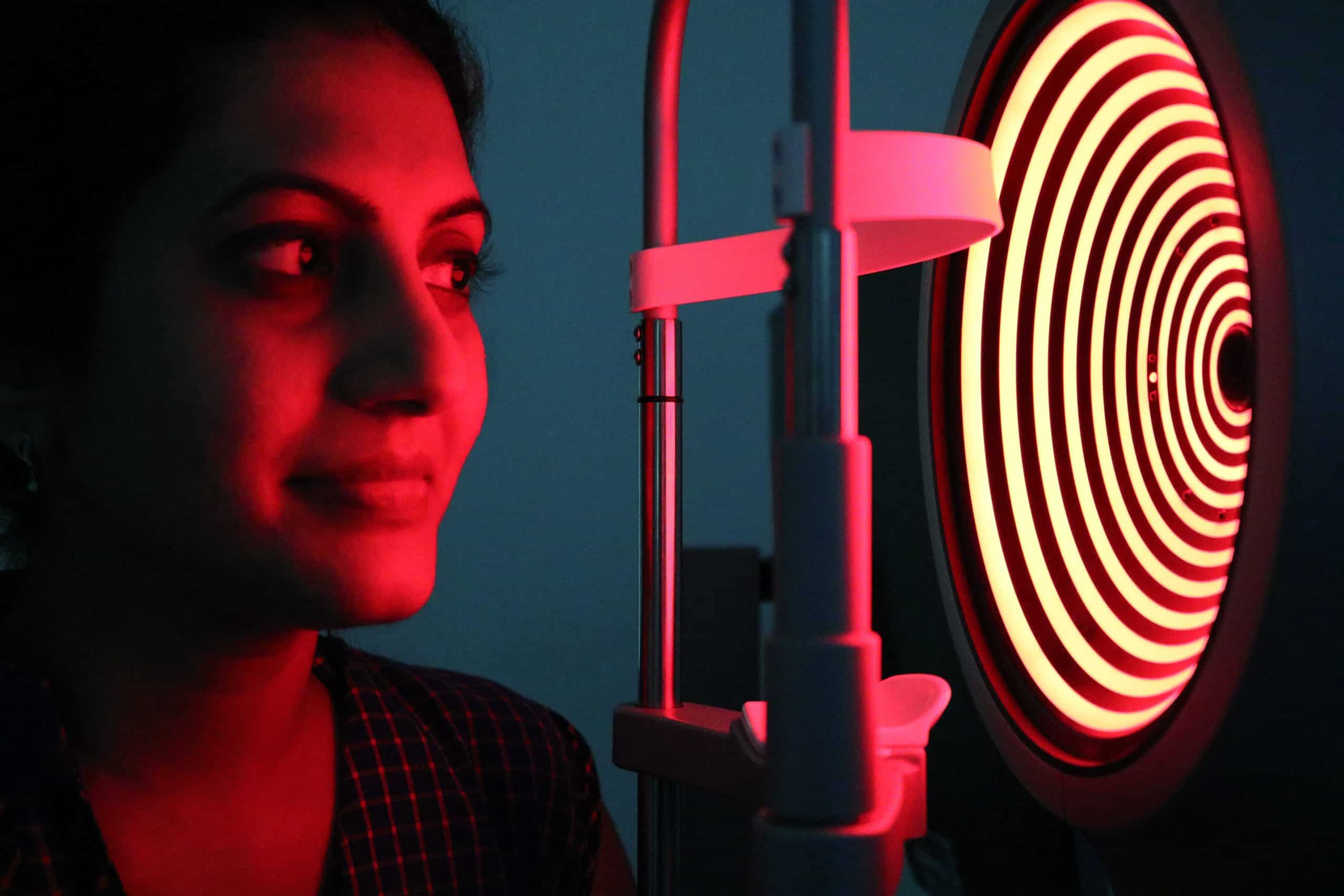
Corneal topography
Corneal topography is a procedure used to monitor and measure changes affecting the strength and integrity of the cornea of your eye. At Narayana Nethralaya, your cornea will undergo detailed evaluation using all the latest topographers available
Pentacam
Works on the principle of a rotating Scheimpflug camera system for anterior segment analysis. An advanced tool for measuring topography and elevation of the anterior and posterior corneal surface and the corneal thickness – in short the most advanced tool for detection and monitoring progress of your disease.

Schwind Sirius Topographer and Planning System
It consists of a combination of two rotating Scheimpflug cameras and a Placido disk, and allows full analysis of the topography and elevation of the anterior and posterior corneal surface and full corneal thickness. An integrated software also helps us plan your laser surgery based on your corneal map.

Galilei & Orbscan
Galilei & Orbscan are other topographers used for Keratoconus evaluation.


Anterior Segment OCT & Epithelial Mapping
Advanced software for point to point mapping of your corneal epithelium (first layer of your cornea) helps us in more accurate planning of the laser procedure along with cross linking.

Corvis ST
Comprehensive biomechanical screening and Keratoconus detection. Helps determine your eye pressure and the overall strength of the eyeball.

Confocal Microscopy
Advanced microscopy technique which enables us to see the ultra microscopic structure of the cornea in just few minutes.

Treatment of Keratoconus
Keratoconus can present at different stages and each stage of disease needs a customized treatment protocol to be followed. In nascent stage of disease vision can be corrected with spectacles and contact lenses.
As the keratoconus progresses more sophisticated lens design is required to rectify the increased irregularity of the corneal surface. Eventually as the disease advances the cornea becomes increasingly thin and buldging which necessitates the need for rigid gas permeable contact lenses for vision correction
At this stage a Cross Linking procedure is usually advised to strengthen your cornea.
Keratoconus
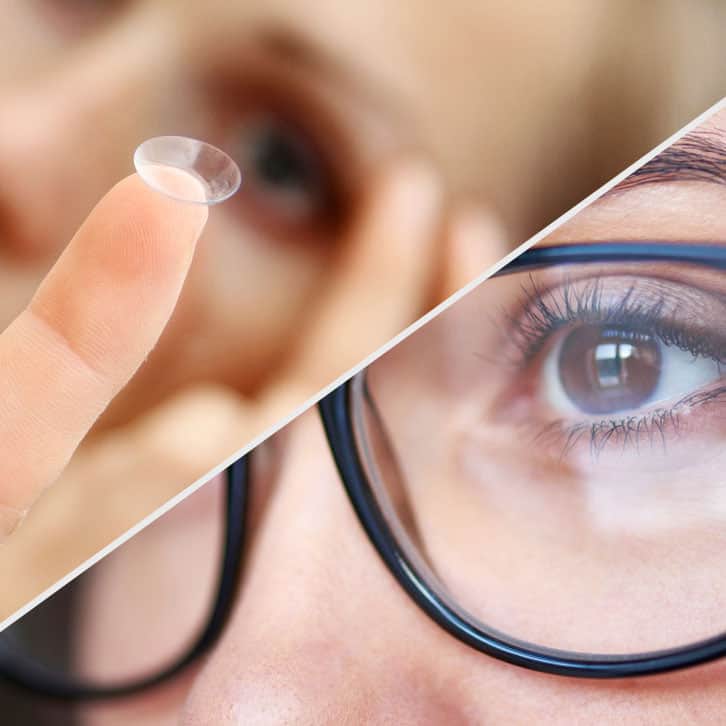
Contact Lenses
Our Specially Trained Optometrists will do a trial and decide which type of Contact Lens best fits over your eye. The contact lenses should be well fitted and would need regular follow up visits to achieve and maintain good vision.
Click here to know more
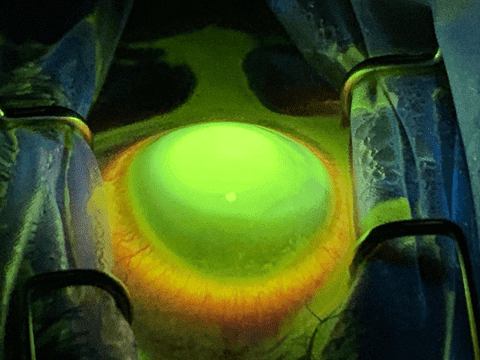
Collagen cross-linking
Collagen Cross Linking is a procedure to stop the progression of Keratoconus which involves removing the skin (epithelium) from the surface of the cornea either manually or by a Laser and custom-made riboflavin eye drops are applied to the cornea every 2 mins for 20 mins. The eye is then exposed to UVA light for 10 minutes.
Click here to know more
Laser Procedures in Keratoconus
Topography-guided photorefractive keratectomy (TPRK) uses a customized excimer laser treatment guided by a topographic map. After the laser ablation, the Cross Linking procedure is performed and then a bandage soft contact lens is placed.
Click here to know more

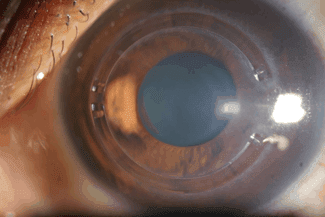
INTACS
INTACS are implantable intracorneal ring segments (ICRS) and INTACS is the trademark name for thin plastic, semi-circular rings inserted into the mid layer of the cornea. Narayana Nethralaya was the first hospital to introduce Intacs in India in 2005 and we have also designed and published a Nomogram for the use of INTACS in Keratoconus which is followed worldwide.
Click here to know more
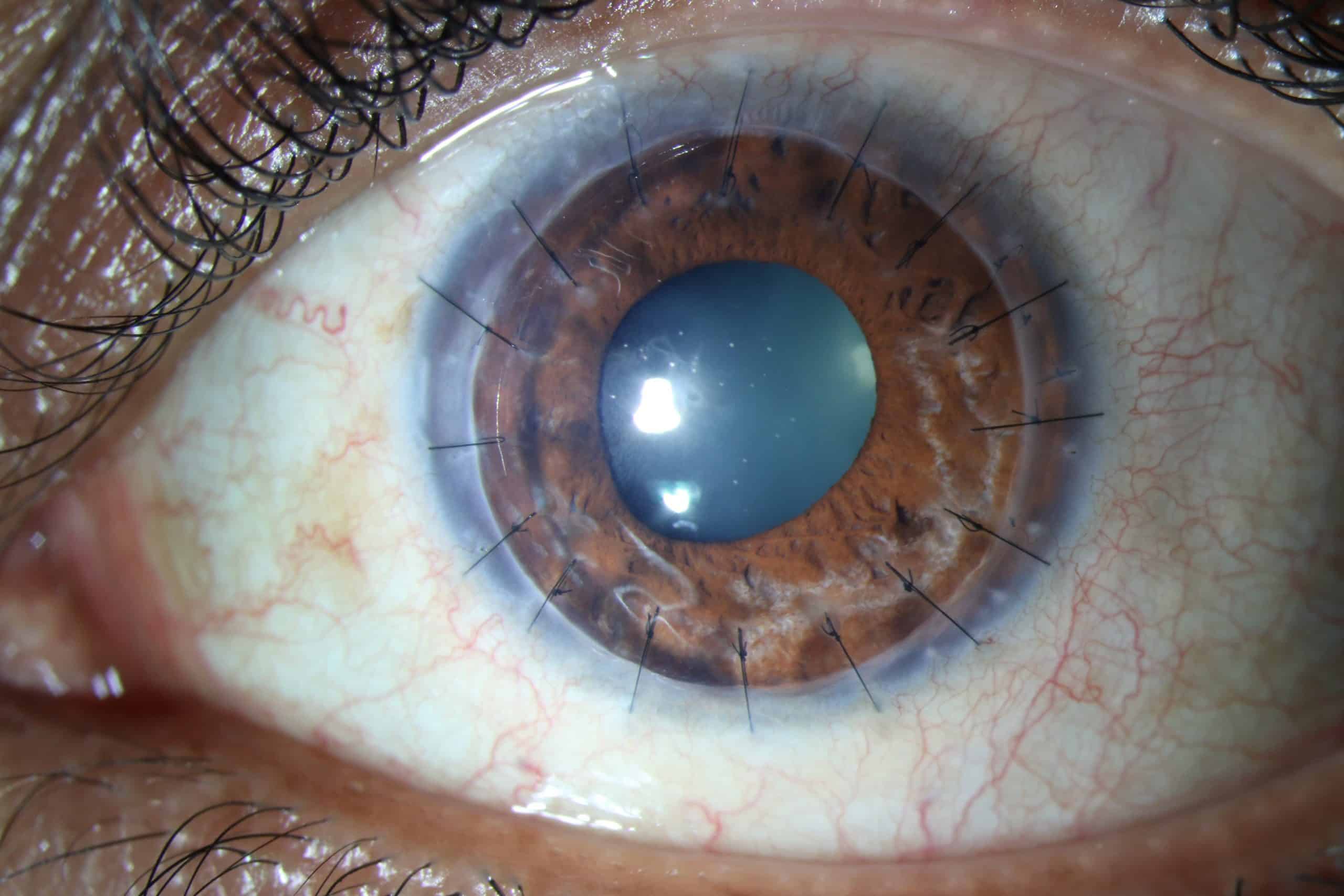
Corneal Transplant Surgery & Visual Rehabilitation
Keratoconus is a condition that requires corneal transplant when the patient has extremely thin cornea or has very low vision which cannot be corrected by rigid contact lenses either due to scarring, steepening of cornea or intolerance to these lens. Mostly the corneal transplant is done on an outpatient basis – so you can leave the hospital or center a few hours after the surgery is done.
Click here to know more
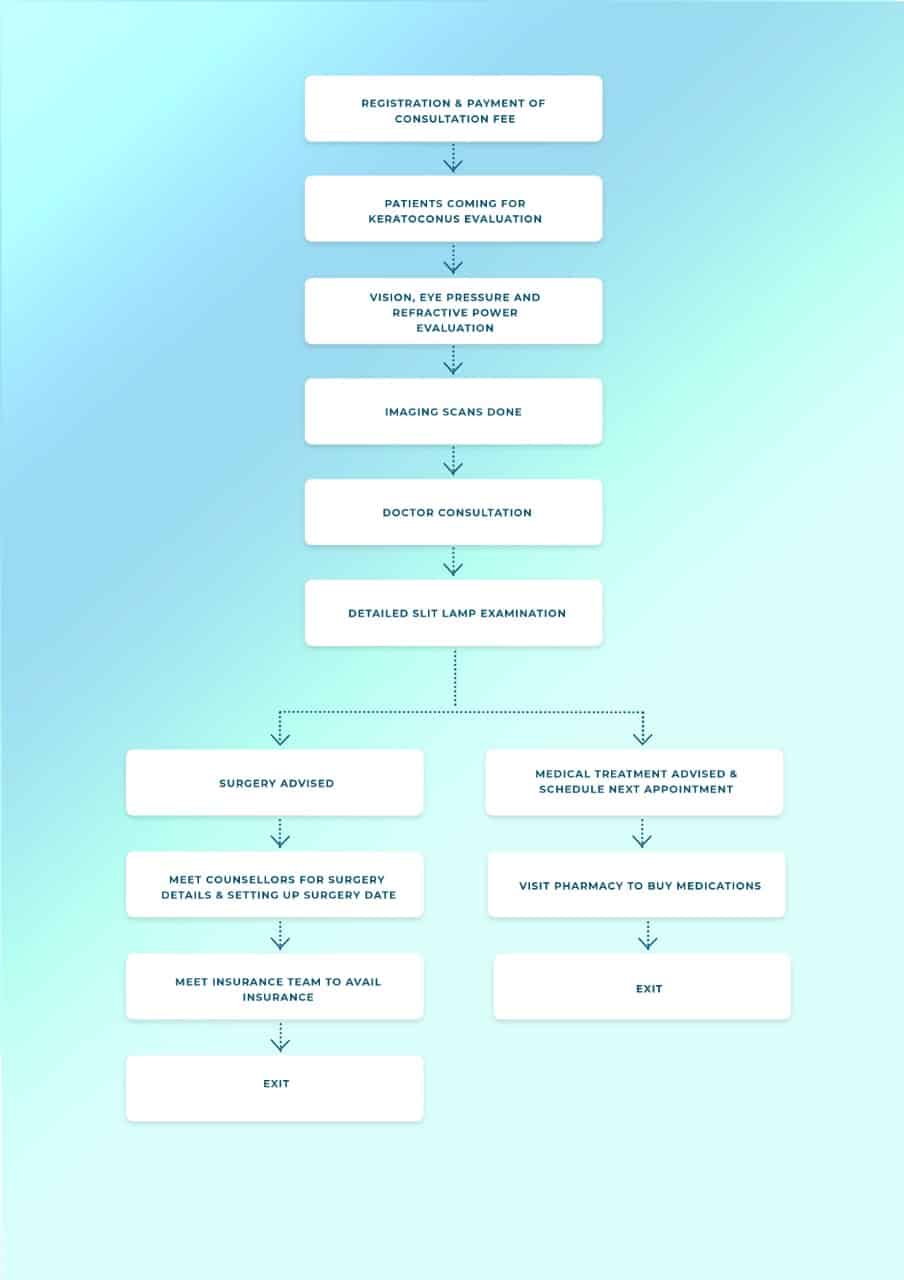
Keratoconus Consultation – Patient Process Flow
If you have light sensitivity, poor night vision, multiple ghost images, frequent change of glasses or contact lenses, blurring and headaches, you should schedule an appointment with an ophthalmologist to get your eyes checked immediately. Your initial consultation with the doctor will approximately take 2 hours if you do not require cross-consultation and up to 4 hours if you require cross-consultation. During your consultation, our doctors and counsellors will determine the best course of action for your visual needs, go over the risks and benefits of treatment, and help you choose the best procedure that is suitable for preserving and improving your vision. We suggest you bring a family member or friend with you to help you with your decision-making.
Now Eye Know Videos
Keratoconus Doctors NN1

Dr. Rohit Shetty
Chairman

Dr. Naren Shetty
Vice Chairman

Dr. Sharon Dsouza
Consultant

Dr. Pooja Khamar
Consultant & Lead Trainer

Dr. Gairik Kundu
Consultant
Keratoconus Doctors NN2

Dr. Himanshu Matalia
Medical Superintendent

Dr. Nandini C
Consultant
Keratoconus Doctors NN3

Dr. Rohit Shetty
Chairman

Dr. Pooja Khamar
Consultant & Lead Trainer

Dr. Shilpa Das
Cornea consultant

Dr. Gairik Kundu
Consultant
Keratoconus Doctors NN4

Dr. Naren Shetty
Vice Chairman

Keratoconus
Case Study 1
KC CASE
A 23 year old boy came to get his glasses changed as he was uncomfortable with his current prescription. On questioning further, we found that this was the 4th time he was changing his glasses that year. He was uncomfortable using contact lenses. On presentation his best corrected visual acuity was 6/12p with -2.50DS/ -6.25DC at 60 degrees in the right eye and 6/9 with -1.50DS/ -3.50DC @ 130 degrees in the left eye. Retinoscopy displayed a scissor reflex in both eyes and pentacam was suggestive of keratoconus in both eyes. He was advised to undergo a topo-guided photorefractive keratectomy with collagen cross linking in his right eye followed by his left eye. Post-operative his best corrected vision improved to 6/6p with glasses. His contact lens fitting improved after the surgery and the patient was satisfied with his treatment result.
Book an appointment with our Keratoconus Team

Keratoconus
Case Study 2
A 24 year old lady presented with itching in both eyes, associated with frequent rubbing. On evaluation, there was presence of follicles in the undersurface of her eyelids. On refraction, her best corrected visual acuity in the right eye was 6/24 with -1.25 DS/ -6.50 DC @75 and in left eye was 6/6 with -2.75 DS/ -2.50 @115. Retinoscopy displayed a scissor reflex in the right eye and Pentacam was suggestive of keratoconus. She was advised INTACS with cross-linking in her right eye. Post-opearative topography showed stable scans and her best corrected visual acuity with contact lens was 6/9P. The patient was happy with her postoperative results.
Book an appointment with our KeratoconusTeam

Keratoconus
Case Study 3
A 30 year old lady presented with diminished vision in both eyes since 6 years. Her vision improved with spectacles and she would wear contact lenses occasionally. On examination her best corrected visual acuity in the right eye was 6/12 p with -5DS / -5.25 DC @ 30 and 6/18p in the left eye with -8 DS/-5.25DC@180. Retinoscopy displayed a scissor reflex in right eye and Pentacam was suggestive of keratoconus. She was advised topo-guided photorefractive keratectomy with cross-linking in her right eye followed by left eye. Post-opearative topography showed stable scans. However, she did not want to wear glasses after her procedure, so an Implantable Collamer Lens (ICL) was planned for her, in both eyes. Following this, her best corrected visual acuity was 6/6p in both eyes and she was very happy with her results.
Book an appointment with our Keratoconus Team
Our patient care philosophy
At Narayana Nethralaya, “Quality of Care” and “Patient Safety” is our priority. Concern for our patients’ well being is at the core of what we do, and what drives us. Four units of Narayana Nethralaya are NABH Accredited – the highest national recognition for quality in patient care and safety. Our Keratoconus team help patients make an informed treatment choice on the type of treatment and surgery that is best suited for their lifestyle. We have an exclusive counseling team to address any doubts or questions that people may have about Keratoconus treatment options and procedures.

Patient Testimonials
At Narayana Nethralaya, we are committed to providing our patients with advanced quality eye care at affordable prices. These eye surgery experiences stand testimony to the excellence in eye care that we offer.