Retinal Vein Occlusion
Retinal vein occlusion is a blockage in the ocular blood vessel that can result in vision loss. The retinal veins carry away used blood from the retina and when one of these veins are blocked, the used blood cannot drain away which causes swelling and hemorrhage (bleeding).
There are two distinct types of retinal occlusion:
Central retinal vein occlusion (CRVO) – a blockage in the main retinal vein.
Branch retinal vein occlusion (BRVO) – a blockage in a smaller retinal vein.
Retinal Vein Occlusion
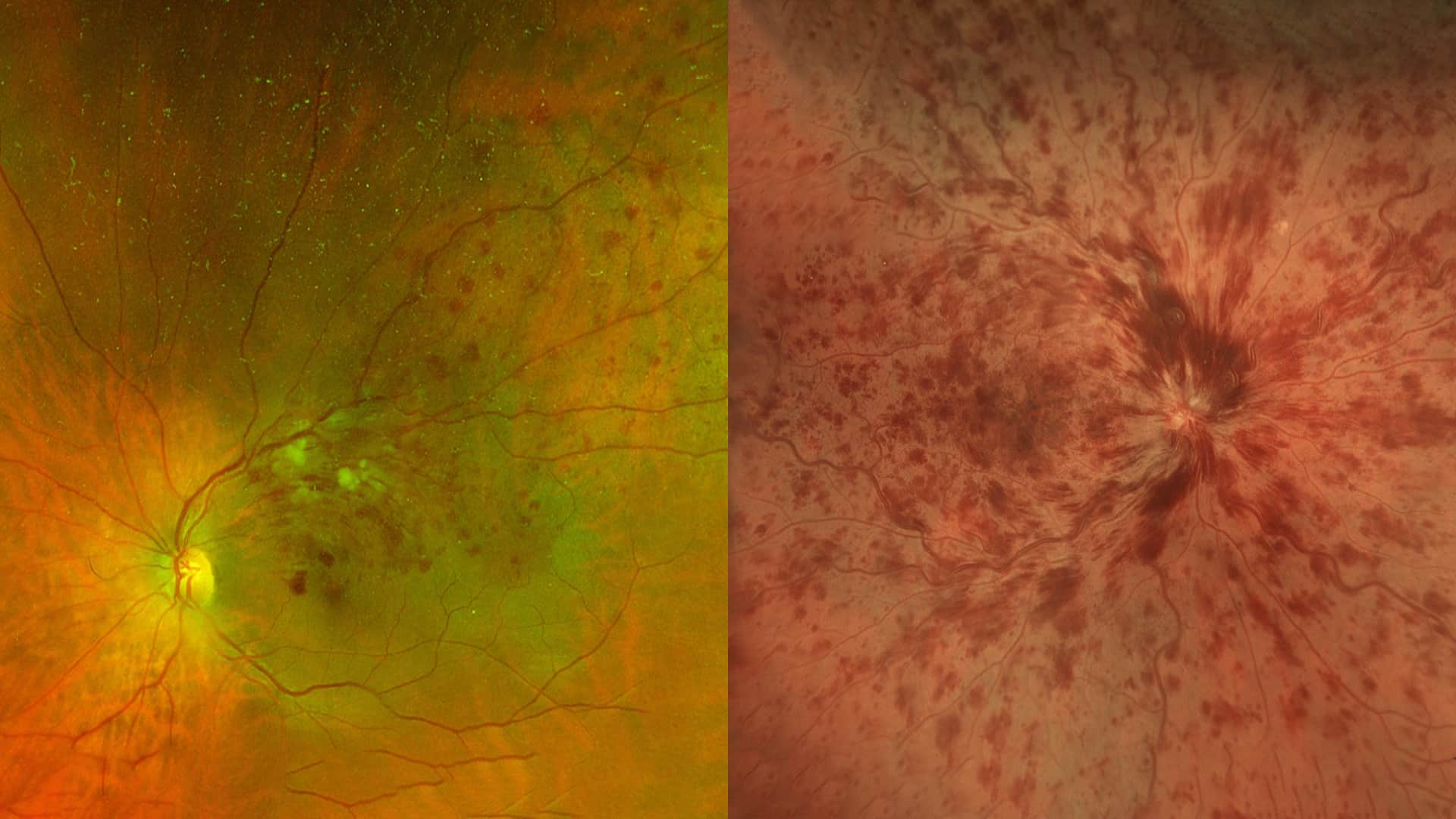
Central retinal vein occlusion (CRVO)
Arteries carry blood from the heart to various body parts, and veins return it. The retina has one major artery and one major vein, which is called the central retinal vein. Sometimes this vein can be blocked suddenly to some degree by a blood clot. In most cases, an underlying cause is not known. It is more common in patients with glaucoma, high blood pressure, arteriosclerosis, and diabetes.
When the central retinal vein is blocked, the circulation through the retina is greatly reduced and often resulting in swelling of the center of the retina which is called macular edema leading to blurring of vision. A few patients have a spontaneous improvement in vision with time. However, in most cases the vision remains the same or worsens without treatment. The ultimate visual outcome cannot be predicted for anyone. In general, the more severe the occlusion and associated macular edema, the less likely the vision will improve spontaneously.
Treatment options for CRVO
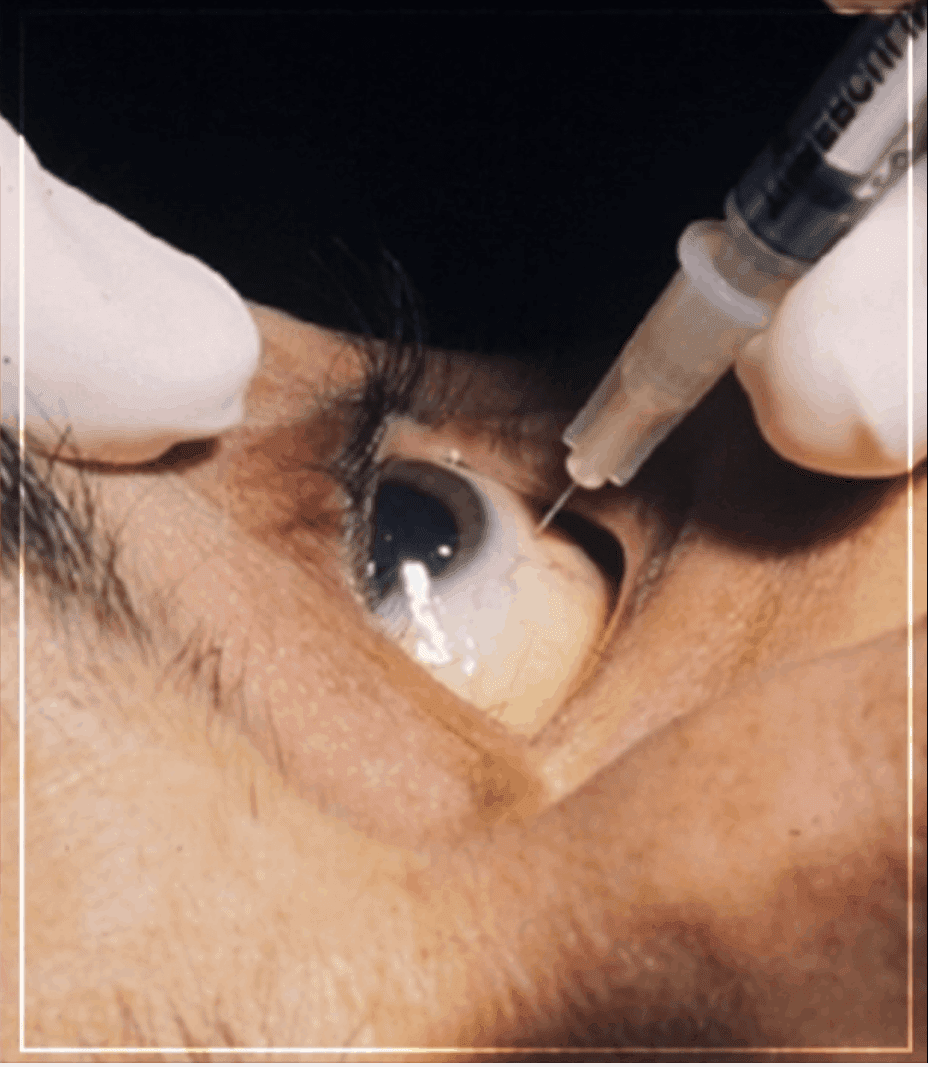
Treatment options proven to be effective in reducing macula edema and improving vision to some degree include medicines injected into the eye such as VEGF blockers (Lucentis and Avastin) and steroids (Triamcinolone and Ozurdex). Eye drops, and glasses do not help to improve vision. Patients with macular edema need ongoing follow-up and regular injections in order to preserve vision. In about one-third of all cases, a severe form of glaucoma called NEOVASCULAR GLAUCOMA develops and the eye pressure can rise to very high levels which necessitates a laser treatment for prevention. Often a VEGF blocker injection into the eye also may be needed. These treatments can help to prevent or control the glaucoma but they do not improve the vision when it is affected by high eye pressure.
There is no reason to limit one’s activities, to avoid reading, to avoid watching TV, etc. However, due to blurring of vision and hampered depth perception one should be very careful doing anything which requires the ability to judge distances such as working around machinery, climbing on ladders and scaffolds, pounding nails, pouring hot liquids, and driving. It is relatively uncommon for a similar process to affect the other eye, and blurry vision in one eye does not in any way harm the “good eye”. A patient should come back sooner than scheduled if there is a marked decrease in vision or if the eye becomes painful.
Branch Retinal Vein Occlusion (BRVO)
BRVO is a blockage of one or more branches of the central retinal vein, which runs through the optic nerve. Branch Retinal Vein Occlusion symptoms include Peripheral vision loss, blurred or distorted central vision and floaters.
It is more common in patients with high blood pressure, diabetes, and atherosclerosis. Smoking is also a significant risk factor. However, in some cases, there is no apparent underlying cause. Underlying medical conditions that are considered associated risk factors such as high blood pressure require evaluation and treatment with a primary care physician.
Stages of branch retinal vein occlusion (BRVO)
Early Stage: Early in the fluorescein angiogram test, the retinal hemorrhages appear dark and the fluorescein dye is slow in filling the superior retinal vein.
Mid Stage: A lack of perfusion of the capillaries can be seen.
Late Stage: The intense cloudy white signal indicates leakage of fluid from the affected retinal vein, which produces macular edema.
With a BRVO, the circulation of blood through the affected vein is either halted or reduced, often resulting in an accumulation of blood and fluid (macular edema) within the retinal tissue. The reduction in blood flow (ischemia) and macular edema both contribute to decreased visual acuity. While gradual spontaneous improvement in vision is possible in a minority of patients, without treatment the vision in most patients will remain decreased or even worsen.

Treatment options for BRVO
While BRVO cannot be cured, there are effective treatments that can help patients maintain or improve their visual outcome by reducing the associated macular edema. Treatment options include intravitreal injection (injection of medicine into the eye) and laser.
Intravitreal injection of vascular endothelial growth factor (VEGF) inhibitors such as Lucentis (FDA approved), Eylea (FDA approved), and Avastin (used off-label) or steroids such as triamcinolone and Ozurdex (FDA approved) can help maintain or improve vision.
Laser is sometimes used to treat macular edema but is now considered a second-line treatment for most cases based on visual outcomes and limitations. For instance, if there is significant hemorrhage in the retina, laser cannot be performed until the hemorrhage resolves spontaneously, which takes few months.
In response to a BRVO, some patients will develop an abnormal growth of fragile new blood vessels (retinal neovascularization) on the surface of the retina months or years after initial diagnosis. These blood vessels generally do not have any associated symptoms unless they rupture and bleed. In general, rupture is spontaneous and unpredictable, and if there is a significant amount of hemorrhage into the vitreous cavity of the eye, vision can be dramatically reduced. Although the blood may resolve spontaneously in some cases, it can take weeks or months depending on the severity. If neovascularization is detected on a follow-up office visit, laser can be administered to shrink the abnormal fragile vessels in order to minimize the risk of vitreous hemorrhage and vision loss. Laser does not guarantee that there will be no future haemorrhaging, but it does significantly lower this risk. Occasionally if there is a very severe or persistent (non-clearing) vitreous hemorrhage, vitrectomy surgery may be warranted to remove the blood.
