Vitreoretinal Surgery
Narayana Nethralaya has fully equipped state of art vitreo retinal surgical suites in each of its branches. The surgeries are performed for a variety of retinal disorders like retinal detachment, advanced diabetic eye disease, vitreous hemorrhage, endophthalmitis, macular hole and epiretinal membrane using the latest small gauge micro incisional vitrectomy system (MIVS). The institute also boasts of having the 3D Ngenuinity visualisation system which allows the surgeon to perform a heads-up vitreoretinal surgery. Also, scleral buckle surgery and pneumatic retinopexy are routinely performed for the management of rhegmatogenous retinal detachment. Complications following anterior segment surgeries like dislocated nucleus and intraocular lens dislocation are managed with the fixing of the scleral fixated or iris-claw intraocular lenses.
Vitreoretinal Surgery
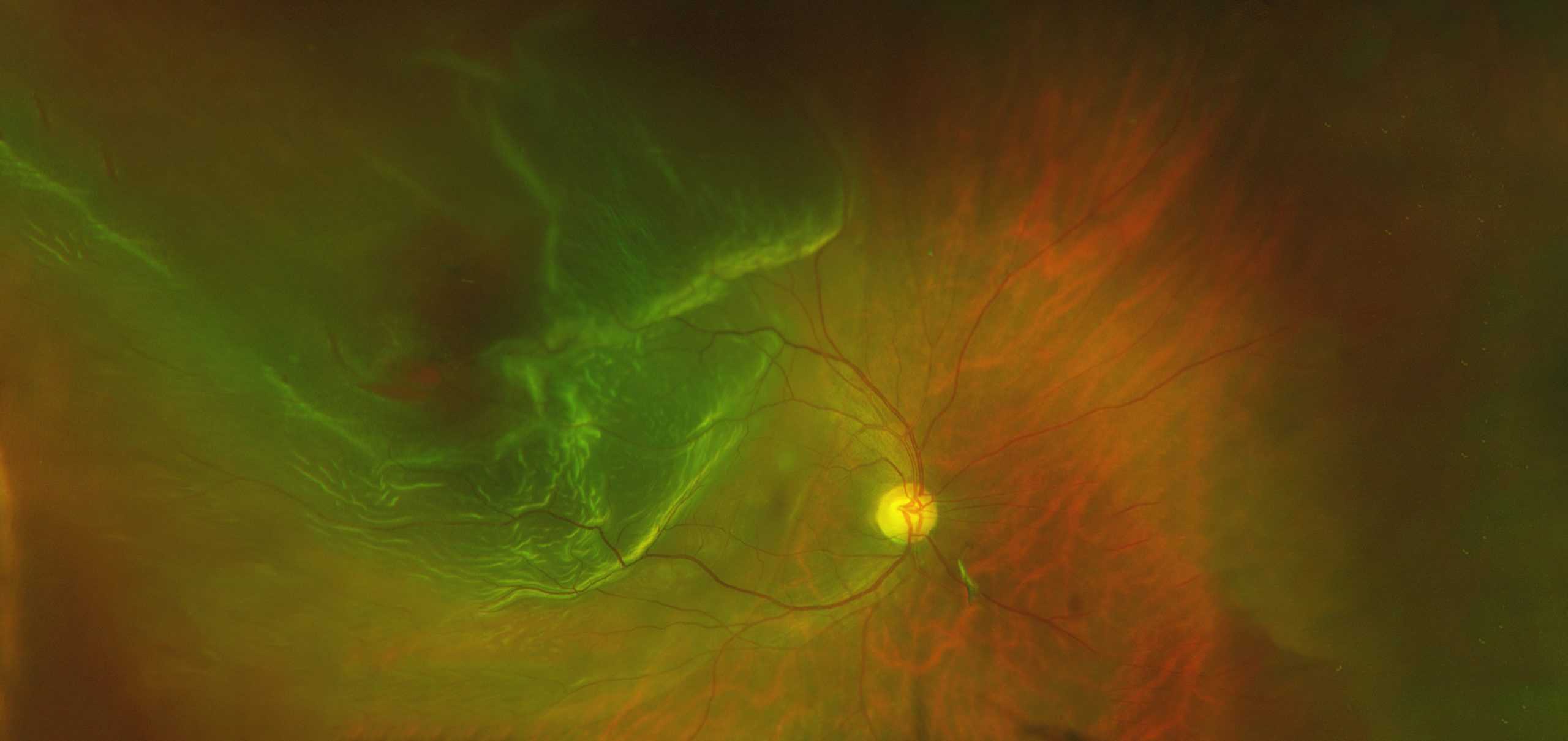
Retinal Detachment
A retinal detachment is a separation of the retinal layers. Over time, retinal detachment will lead to progressive loss of peripheral and, eventually, central vision. Left untreated, total and permanent loss of sight eventually occurs in most cases.
A rhegmatogenous type of retinal detachment which is the most common type is caused by a break, tear or hole in the retina, allowing fluid from the vitreous cavity of the eye to go under the retina, detaching it from the eye wall. Retinal tears and associated detachments of the retina are often spontaneous and unpredictable events. While detachment can arise following trauma, it is usually caused by separation of the vitreous gel from the retina. Over time as we age, the vitreous gel liquefies. It eventually collapses upon itself and separates from the surface of the retina (posterior vitreous detachment). During or shortly after this event, a retinal tear can occur as a result of the gel pulling on the thin retinal tissue.
Risk factors for developing retinal tears and detachment include myopia (near-sightedness), particularly thin patches within the peripheral retina (lattice degeneration), family history, previous eye surgery, and trauma.
The rate of progression of a retinal detachment can vary from days to weeks depending on many factors such as patient age as well as the size and the number of retinal tears.
Symptoms of vitreous detachment, retinal tear, and retinal detachment may coexist and include:
- Sudden onset of floaters (mobile blackspots or cobwebs in the vision)
- Sudden onset of flashing lights in vision
Blurred vision
Gradual loss of peripheral vision in the form of a shadow, curtain, or cloud (this corresponds to the retina detaching)
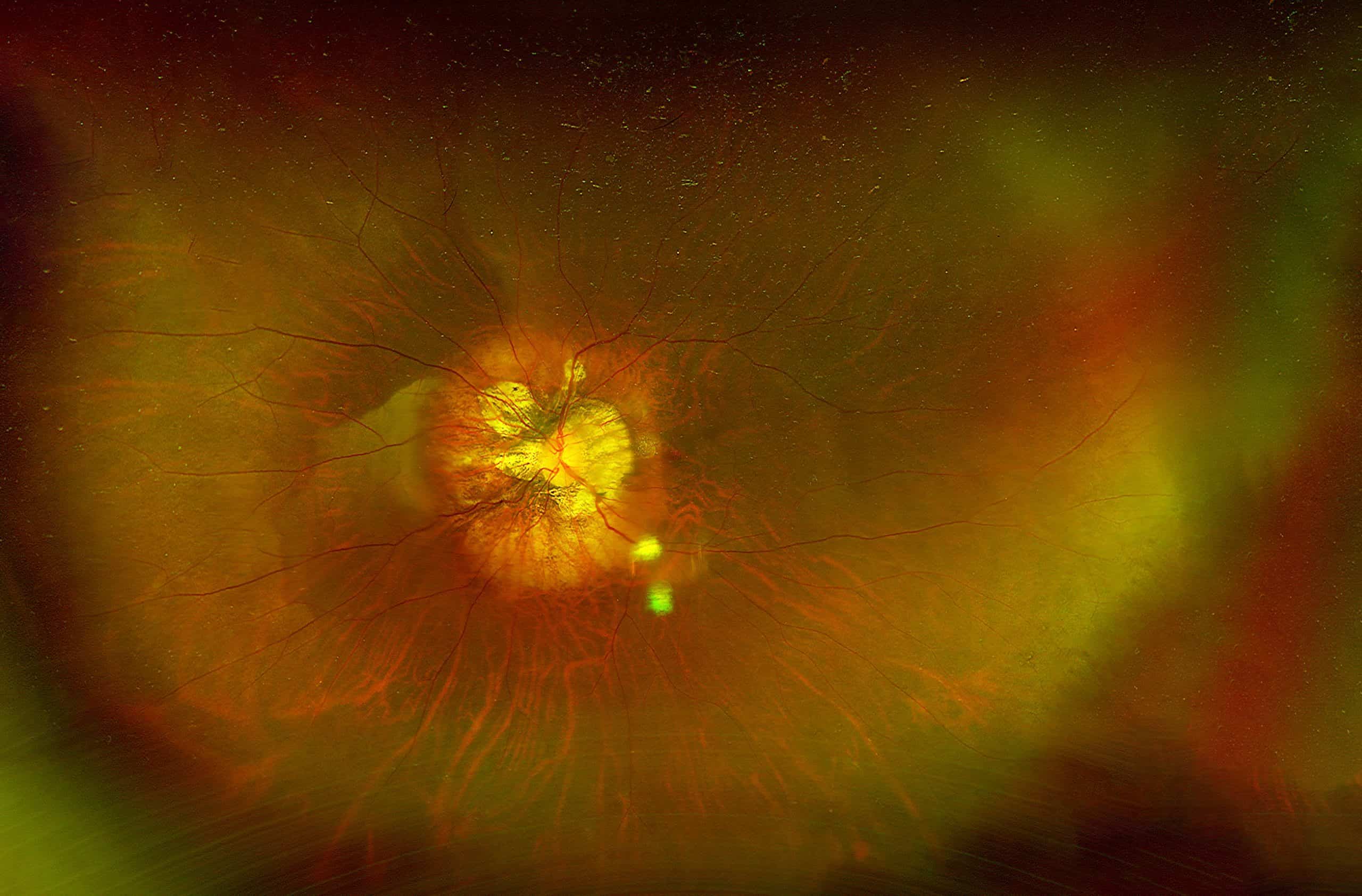
Examination – A comprehensive ophthalmic examination is essential to diagnose and treat a retinal detachment. Through a dilated pupil, the ophthalmologist will see one or more tears in the retina with varying amounts of underlying fluid. There may also be some degree of vitreous hemorrhage, which occurs when a retinal tear involves a retinal blood vessel.
Retinal detachments often cause some degree of permanent visual field or central visual acuity loss, even after successful reattachment. Final visual outcomes are best if the detachment is detected and treated before it involves the center of the retina (macula). A change of eyeglasses after retinal detachment surgery may or may not improve vision. Longstanding retinal detachments or those with associated scar tissue (proliferative vitreoretinopathy) typically have a poor visual prognosis.
Treatment and how to prevent retinal detachment – If a retinal hole or tear is detected before there is retinal detachment, laser or cryotherapy (freezing treatment) to the retinal tear is often successful in sealing the retinal defect, preventing a retinal detachment. However, if a retinal detachment has already developed, a retinal reattachment procedure is typically necessary.

