Corneal Transplant Surgery & Visual Rehabilitation
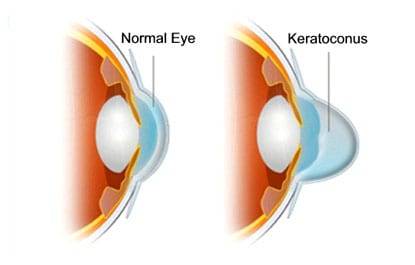
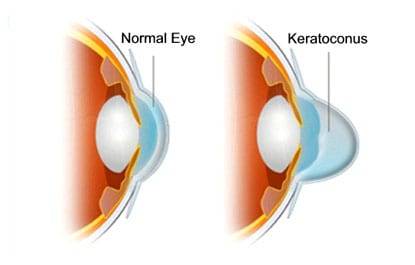
Keratoconus is a condition that requires corneal transplant when the patient has extremely thin cornea or has very low vision which cannot be corrected by rigid contact lenses either due to scarring, steepening of cornea or intolerance to these lens. Mostly the corneal transplant is done on an outpatient basis – so you can leave the hospital or center a few hours after the surgery is done.
Keratoconus
Types of Corneal Transplantation Surgery
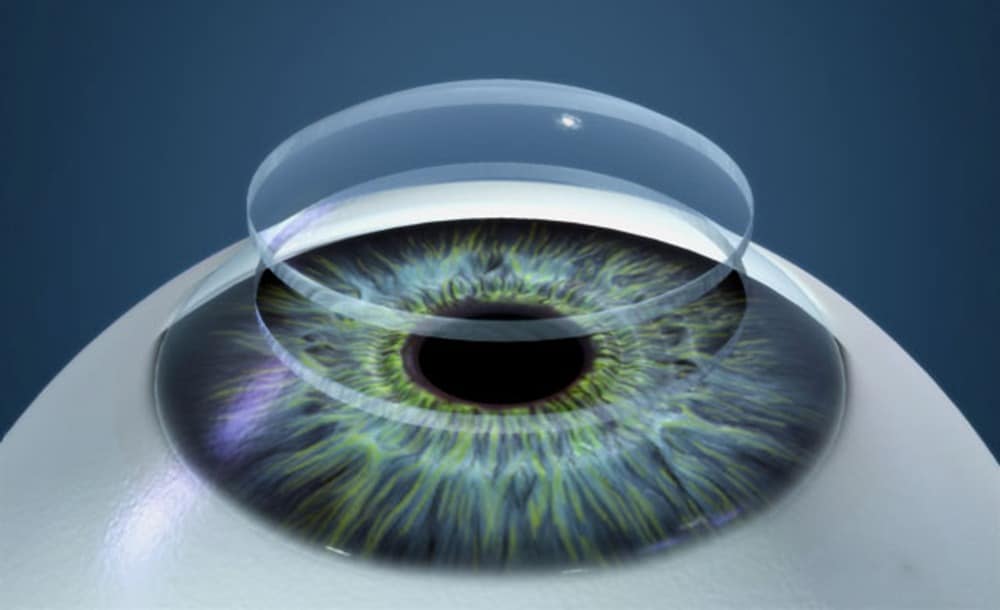
Deep Anterior Lamellar Keratoplasty
Partial corneal transplant in which the anterior diseased layers of the patient’s cornea are removed and replaced with the same layers from a healthy donor cornea. There are less chances for corneal graft rejection or failure and requires less recovery.
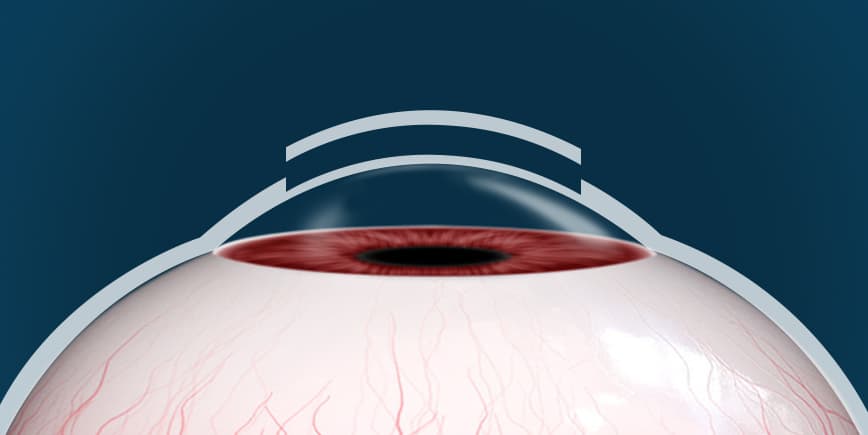
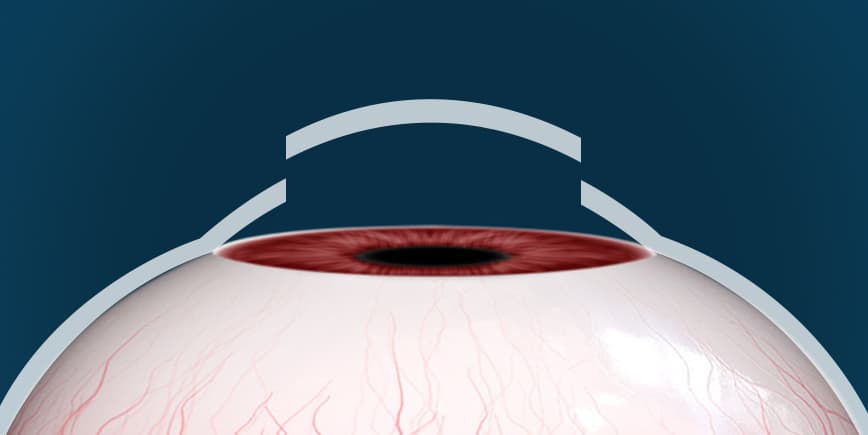
Penetrating Keratoplasty
Full thickness Corneal Transplant in which all layers of the patient’s cornea are replaced by a donor cornea. This is undertaken when the disease is sufficiently advanced with scarring, so as to preclude a lamellar or partial transplant.
Steps of Penetrating Keratoplasty
- Local or general anaesthesia can be used for this procedure. The entire procedure is done under sterile conditions under a microscope. A trephine (circular cutter like instrument) is used to remove the diseased cornea.
- The area of diseased cornea is measured and a “button” of the size of the diseased cornea is cut from the donor cornea and then sewn in place with very fine nylon sutures. A patch and shield are then placed to protect the eye.
- After surgery, rest is advised. Generally there is very little pain which is usually relieved by painkillers.
- Once the patch is removed, it is imperative to protect the operated eye from any forms of accidents.
- Postoperative care is by far the most time-consuming and the most important part of the surgery. Care must be taken to avoid direct trauma to the eye as a new cornea has been sutured in place. Contact sports are discouraged after corneal transplant, however, normal activity can be resumed within a few days.
- Sutures are normally left in place in case of good vision, but may be removed after three months. No discomfort arises as these sutures are buried. They can be removed or adjusted after surgery to improve quality of vision. • To prevent rejection of the new cornea, steroid eye drops are used for several months after surgery which low dosage steroids may be continued indefinitely depending on the condition. No side effects arise from the steroid drops, unlike oral steroids.
- Any symptoms of floaters, sudden blurring of vision, loss of peripheral vision, redness, sensitivity to lights, vision loss or pain must be reported immediately (including weekends, evenings or holidays).
Visual Rehabilitation after a Transplant
Vision may continue to change for many months, even upto a year to get good stable vision. Visual recovery is usually faster with DALK compared to a penetrating Keratoplasty. Most stable vision usually occurs after all sutures are removed, which occurs at different times for different patients. The majority of Keratoconus patients have their sutures removed 12 months after surgery.
Scope of Visual Recovery
A small percentage of transplant patients obtain good uncorrected vision that does not require contact lens or glasses but majority of cases, some kind of vision correction may be needed after surgery.

Follow up schedule after surgery
What to Expect at Every Visit
Day 0: After Surgery, you will be examined by a doctor and medications, precautions will be explained in detail. Day 1: A doctor will examine your eye and post surgical healing
Day 3 / 4: Your Bandage Contact Lens will be removed by your doctor. Additonal eyedrops will then be started for your operated eye.
Day 10: On this check up, the doctor will monitor your healing post surgery. This follow up is essential to monitor your intra ocular pressure (eye pressure) after surgery.
Day 30 (1 month): On this follow up, after checking the post surgical healing progress, your doctor will advise some corneal scans for you. This is to monitor the thickness and shape of the cornea post surgery. Your eye pressure will also be checked.
Day 90 (3 months): This is an important visit for Visual Rehabilitation. Your glass power will be checked and temporary glasses will be prescribed to you. Corneal Scans will be repeated to monitor the disease in your other eye as well as operated eye. If required, surgery will be advised for your other eye. 6 months: Your Glass Power will be re checked & if desired a contact lens trial can be undertaken at this visit. Contact Lenses can be prescribed for both eyes if disease is stable in other eye. At this & every subsequent 6 monthly visit, corneal scans will be repeated to monitor the disease in your other eye as well as the operated eye. If required, surgery will be advised for your other eye. If at any time point, you experience sudden blurring / clouding of vision, redness in both eyes, please visit us immediately. A doctor will examine you and do the needful.